Biphenotypic Sinonasal Sarcoma
Biphenotypic Sinonasal Sarcoma is a newly recognized, very rare, low grade malignant tumor of the nasal cavity which formerly was probably included in fibrosarcoma and synovial sarcoma cases. It is newly recognized by the World Health Organization Classification of Head and Neck Tumours.
Classification
Abbreviations
- Biphenotypic sinonasal sarcoma (BSNS)
- Original name: Low-grade sinonasal sarcoma with neural and myogenic features (LGSSNMF),[1] but it is no longer recommended.
Definitions
- A low-grade spindle cell neoplasm of the sinonasal tract associated with overlying respiratory epithelium and showing S100 protein and actin immunoreactivity.
Signs and Symptoms
The tumor will often affect multiple sites within the upper aerodigestive tract, frequently showing extension into the orbit (25%) or through the cribriform plate (11%) of the ethmoid sinus into the skull base. The patient present with non-specific findings, including difficulty breathing, facial pressure, congestion, pain, and mild epiphora. Often concurrent benign sinonasal tract inflammatory polyps will be seen.
Pathology findings
Microscopic
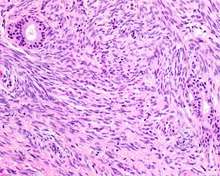
* Infiltrative, highly cellular spindled cell neoplasm that is poorly circumscribed and unencapsulated. Bone destruction or invasion is common. The cells show medium to long fascicles, with a herringbone pattern. The cells are remarkably uniform with elongated nuclei. There are delicate strands of intercellular collagen without ropy or dense deposition. There is a very characteristic concurrent surface-type respiratory epithelial proliferation invaginated from the surface or in small cystic spaces within proliferation, often forming glands.
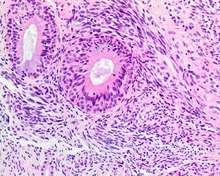
The background may have a rich vascularity and usually has a small number of scattered lymphocytes. Mitoses are rare, while necrosis, ulceration and hemorrhage are usually absent.
Ancillary Tests
- S100 protein: Focal, patchy to diffuse in all tumors.
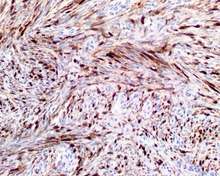 S100 protein reaction in a biphenotypic sinonasal sarcoma.
S100 protein reaction in a biphenotypic sinonasal sarcoma. - Smooth muscle actin or muscle specific actin seen in nearly all tumors, but strong and diffuse reaction with SMA is seen in only about 50% of cases.
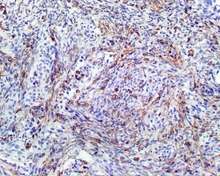 Smooth muscle actin reaction in a biphenotypic sinonasal sarcoma.
Smooth muscle actin reaction in a biphenotypic sinonasal sarcoma. - No reactivity with SOX10, myogenin, estrogen receptor, progesterone receptor or keratins.
Genetic Testing
- t(2;4)(q35;q31.1): PAX3-MAML3 fusion protein.[2] Only a few cases have shown a PAX3-NCOA1 (inv(2)(q35p23)), and the tumor is negative for SS18-SSX1 or SSX2
Differential diagnoses
- Fibrosarcoma: Can be very similar; although, fascicles and herringbone pattern tend to be longer and more well developed
- Synovial Sarcoma: Almost histologically identical, but FISH or RT-PCR would show characteristic translocation (SS18-SSX1 or SSX2).
- Malignant Peripheral Nerve Sheath Tumor, Including Triton Tumor: Distinctive alternating light and dark cellular areas; association with peripheral nerves; usually a high-grade tumor with pleomorphism, necrosis, and increased mitoses. Generally shows reactivity with S100 protein and SOX10 while negative: SMA, MSA
- Leiomyosarcoma: Fascicular architecture, with cigar-shaped nuclei showing blunt ends, perinuclear halos, and eosinophilic cytoplasm. Much stronger reactivity with desmin and SMA, while usually negative with S100 protein.
- Mucosal Melanoma: this is also a spindled cell tumor in many cases, but there is pleomorphism, intranuclear inclusions and prominent nucleoli. The neoplastic cells are usually strongly reactive with S100 protein, SOX10, HMB45, Melan-A, tyrosinase, while negative for SMA, MSA.
Epidemiology
A very rare tumor, although as it is newly described, probably is under reported. Patients present over a wide age range (24–85 years), with a mean age of 52 years. There is a female predominance (F:M 3:1).
Management
- Surgery, often accompanied by radiation is the treatment of choice. There is frequent (44%) local recurrence, but often many years after the initial presentation. Up to now, there are no regional or distant metastases reported, and no patient has yet died from disease.[1]
References
- 1 2 Lewis JT, Oliveira AM, Nascimento AG, Schembri-Wismayer D, Moore EA, Olsen KD, Garcia JG, Lonzo ML, Lewis JE (April 2012). "Low-grade sinonasal sarcoma with neural and myogenic features: a clinicopathologic analysis of 28 cases". Am J Surg Pathol. 36 (4): 517–25. doi:10.1097/PAS.0b013e3182426886. PMID 22301502.
- ↑ Wang X, Bledsoe KL, Graham RP, Asmann YW, Viswanatha DS, Lewis JE, Lewis JT, Chou MM, Yaszemski MJ, Jen J, Westendorf JJ, Oliveira AM (July 2014). "Recurrent PAX3-MAML3 fusion in biphenotypic sinonasal sarcoma". Nat Genet. 46 (7): 666–8. doi:10.1038/ng.2989. PMC 4236026
 . PMID 24859338.
. PMID 24859338.