Chronic venous insufficiency
| Chronic venous insufficiency | |
|---|---|
|
Mild chronic venous insufficiency | |
| Classification and external resources | |
| Specialty | cardiology |
| ICD-10 | I87.2 |
| ICD-9-CM | 459.81 |
| DiseasesDB | 13734 |
| MedlinePlus | 000203 |
| eMedicine | article/461449 |
| MeSH | D014689 |
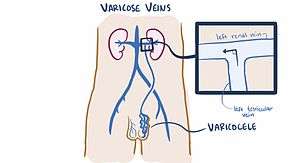
Chronic venous insufficiency (CVI) is a medical condition in which the veins cannot pump enough blood back to the heart.[1] The most common cause of CVI is superficial venous reflux which is a treatable condition.[2] As functional venous valves are required to provide for efficient blood return from the lower extremities, this condition typically affects the legs. If the impaired vein function causes significant symptoms, such as swelling and ulcer formation, it is referred to as chronic venous disease. CVI includes varicose veins and superficial venous reflux ("hidden varicose veins")[3] It is sometimes called chronic peripheral venous insufficiency and should not be confused with post-thrombotic syndrome in which the deep veins have been damaged by previous deep vein thrombosis.
Most cases of CVI can be improved with treatments to the superficial venous system or stenting the deep system. Varicose veins for example can now be treated by local anesthetic endovenous surgery.
The prevalence of CVI is far higher in women than in men.[4][5] The Tampere study, which examined the epidemiology of varicose veins in a large cohort of 3284 men and 3590 women, demonstrated that the prevalence of varicose veins in men and women was 18% and 42%, respectively. The condition has been known since ancient times and Hippocrates used bandaging to treat it.
Signs and symptoms

Signs and symptoms of CVI in the leg include the following:
- Varicose veins
- Itching (pruritus)
- Hyperpigmentation
- Phlebetic lymphedema[6]
- Chronic swelling of the legs and ankles
- Venous ulceration
CVI in the leg may cause the following:
- Venous stasis
- Ulcers.[7]
- Stasis dermatitis,[7] also known as varicose eczema
- Contact dermatitis.[7] Patients with venous insufficiency have a disrupted epidermal barrier, making them more susceptible than the general population to contact sensitization and subsequent dermatitis.
- Atrophie blanche.[7] This is an end point of a variety of conditions, appears as atrophic plaques of ivory white skin with telangiectasias. It is a late sequelae of lipodermatosclerosis where the skin has lost its nutrient blood flow.
- Lipodermatosclerosis.[7] This is an indurated plaque in the medial malleolus.
- Malignancy.[7] Malignant degeneration is a rare but important complication of venous disease since tumors which develop in the setting of an ulcer tend to be more aggressive.
- Pain.[7] Pain is a feature of venous disease often overlooked and commonly undertreated.
- Anxiety.[7]
- Depression.[7]
- Inflammation
- Discoloration
- Skin thickening
- Cellulitis
Causes
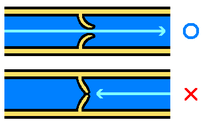
CVI in the leg may be caused by the following:
- Blood clots in the deep veins. This is called Deep vein thrombosis, or DVT. CVI caused by DVT may be described as postthrombotic syndrome
- Arteriovenous fistula (an abnormal connection or passageway between an artery and a vein).
- Phlebitis
- Thrombophilia
- Obesity
- May–Thurner syndrome. This is a rare condition in which blood clots occur in the iliofemoral vein due to compression of the blood vessels in the leg. The specific problem is compression of the left common iliac vein by the overlying right common iliac artery. Many May-Thurner compressions are overlooked when there is no blood clot. More and more of them get nowadays diagnosed and treated (by stenting) due to advanced imaging techniques.
Management
Surgical treatment of CVI attempts a cure by physically changing the veins with incompetent valves. Surgical treatments for CVI include the following:
- Linton procedures (an older treatment)
- Ligation.[8] Tying off a vein to prevent blood flow
- Vein stripping.[8] Removal of the vein.
- Surgical repair.[8]
- Endovenous Laser Ablation
- Vein transplant.[8]
- Subfascial endoscopic perforator surgery.[8] Tying off the vein with an endoscope.
- Valve repair (experimental)
- Valve transposition (experimental)
- Hemodynamic surgeries.
Treatment of CVI in the leg involves managing the symptoms (and preventing the symptoms getting worse) instead of effecting a cure. It is sometimes called conservative treatment. Conservative treatments include:
- Manual compression lymphatic massage therapy
- Skin lubrication
- Sequential compression pump
- Ankle pump
- Compression stockings
- Blood pressure medicine,
- Frequent periods of rest elevating the legs above the heart level
- Tilting the bed so that the feet are above the heart. This may be achieved by using a 20 cm (7-inch) bed wedge or sleeping in a 6 degree Trendelenburg position. Obese or pregnant patients might be advised by their physicians to forgo the tilted bed.
See also
References
- ↑ "Chronic Venous Insufficiency". Society for Vascular Surgery. December 1, 2009.
- ↑ Whiteley MS (2011). "Understanding Venous Reflux - the cause of varicose veins and venous leg ulcers". Whiteley Publishing. Retrieved January 8, 2015.
- ↑ RT Eberhardt; JD Raffetto (2005). "Contemporary Reviews in Cardiovascular Medicine - Chronic Venous Insufficiency. Circulation. 2005 111: 2398-2409 doi: 10.1161/01.CIR.0000164199.72440.08". Circulation. Retrieved January 8, 2015.
- ↑ Evans CJ, Fowkes FG, Ruckley CV, Lee AJ (1999). "Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh Vein Study.J Epidemiol Community Health. 1999 Mar;53(3):149-53.". J Epidemiol Community Health. Retrieved January 8, 2015.
- ↑ Robertson LA, Evans CJ, Lee AJ, Allan PL, Ruckley CV, Fowkes FG (May 2014). "Incidence and risk factors for venous reflux in the general population: Edinburgh Vein Study. Eur J Vasc Endovasc Surg. 2014 Aug;48(2):208-14. doi: 10.1016/j.ejvs.2014.05.017. Epub 2014 Jun 18.". Eur J Vasc Endovasc Surg. Retrieved January 8, 2015.
- ↑ Avril, Stéphane; Badel, Pierre; Dubuis, Laura; Rohan, Pierre-Yves; Debayle, Johan; Couzan, Serge; Pouget, Jean-Fraçois (January 25, 2012). Gefen, Amit, ed. Patient-Specific Modeling in Tomorrow's Medicine. Springer. p. 220. ASIN B00A9YFUDO. Retrieved August 2015. Check date values in:
|access-date=(help) - 1 2 3 4 5 6 7 8 9 Barron GS, Jacob SE, Kirsner RS (Sep 2007). "Dermatologic complications of chronic venous disease: medical management and beyond". Ann Vasc Surg. 21 (5): 652–62. doi:10.1016/j.avsg.2007.07.002. PMID 17823046.
- 1 2 3 4 5 "Chronic Venous Insufficiency". hopkinsmedicine.org.
