Dental restoration
| Dental restoration | |
|---|---|
| Intervention | |
| ICD-9-CM | 23.2-23.4 |
A dental restoration or dental filling is a dental restorative material used to restore the function, integrity and morphology of missing tooth structure. The structural loss typically results from caries or external trauma. It is also lost intentionally during tooth preparation to improve the aesthetics or the physical integrity of the intended restorative material. Dental restoration also refers to the replacement of missing tooth structure that is supported by dental implants.
Dental restorations can be divided into two broad types: direct restorations and indirect restorations. All dental restorations can be further classified by their location and size. A root canal filling is a restorative technique used to fill the space where the dental pulp normally resides.
Tooth preparation

Restoring a tooth to good form and function requires two steps, (1) preparing the tooth for placement of restorative material or materials, and (2) placement of restorative material or materials.
The process of preparation usually involves cutting the tooth with special dental burrs, to make space for the planned restorative materials, and to remove any dental decay or portions of the tooth that are structurally unsound. If permanent restoration can not be carried out immediately after tooth preparation, temporary restoration may be performed.
The prepared tooth, ready for placement of restorative materials, is generally called a tooth preparation. Materials used may be gold, amalgam, dental composites, glass ionomer cement, porcelain or any number of other materials.
Preparations may be intracoronal or extracoronal.
- Intracoronal preparations are those preparations which serve to hold restorative material within the confines of the structure of the crown of a tooth. Examples include all classes of cavity preparations for composite or amalgam, as well as those for gold and porcelain inlays. Intracoronal preparations are also made as female recipients to receive the male components of Removable partial dentures.
- Extracoronal preparations are those preparations which serve as a core or base upon which or around which restorative material will be placed to bring the tooth back into a functional or aesthetic structure. Examples include crowns and onlays, as well as veneers.
In preparing a tooth for a restoration, a number of considerations will come into play to determine the type and extent of the preparation. The most important factor to consider is decay. For the most part, the extent of the decay will define the extent of the preparation, and in turn, the subsequent method and appropriate materials for restoration.
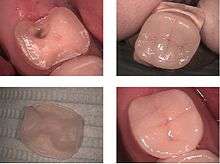
Another consideration is unsupported tooth structure. In the photo at right, unsupported enamel can be seen where the underlying dentin was removed because of infiltrative decay. When preparing the tooth to receive a restoration, unsupported enamel is removed to allow for a more predictable restoration. While enamel is the hardest substance in the human body, it is particularly brittle, and unsupported enamel fractures easily.
Direct restorations
This technique involves placing a soft or malleable filling into the prepared tooth and building up the tooth before the material sets hard. The advantage of direct restorations is that they usually set quickly and can be placed in a single procedure. Since the material is required to set while in contact with the tooth, limited energy can be passed to the tooth from the setting process without damaging it. Where strength is required, especially as the fillings become larger, indirect restorations may be the best choice in some cases.
Indirect restorations
In this technique the restoration is fabricated outside of the mouth using the dental impressions of the prepared tooth. Common indirect restorations include inlays and onlays, crowns, bridges, and veneers. Usually a dental technician fabricates the indirect restoration from records the dentist has provided of the prepared tooth. The finished restoration is usually bonded permanently with a dental cement. It is often done in two separate visits to the dentist. Common indirect restorations are done using gold or ceramics.
While the indirect restoration is being prepared, a provisory/temporary restoration is sometimes used to cover the prepared part of the tooth, which can help maintain the surrounding dental tissues.
Removable dental prostheses (mainly dentures) are considered by some to be a form of indirect dental restoration, as they are made to replace missing teeth. There are numerous types of precision attachments (also known as combined restorations) to aid removable prosthetic attachment to teeth, including magnets, clips, hooks and implants which could be seen as a form of dental restoration.
The CEREC method is a chairside CAD/CAM restorative procedure. An optical impression of the prepared tooth is taken using a camera. Next, the specific software takes the digital picture and converts it into a 3D virtual model on the computer screen. A ceramic block that matches the tooth shade is placed in the milling machine. An all-ceramic, tooth-colored restoration is finished and ready to bond in place.
Another fabrication method is to import STL and native dental CAD files into CAD/CAM software products that guide the user through the manufacturing process. The software can select the tools, machining sequences and cutting conditions optimized for particular types of materials, such as titanium and zirconium, and for particular prostheses, such as copings and bridges. In some cases, the intricate nature of some implants requires the use of 5-axis machining methods to reach every part of the job.[1]
Restoration classifications
Greene Vardiman Black classified the fillings depending on their size and location.[2]
- Class I Caries affecting pit and fissure, on occlusal, buccal, and lingual surfaces of posterior teeth, and palatal of maxillary incisors.
- Class II Caries affecting proximal surfaces of molars and premolars.
- Class III Caries affecting proximal surfaces of centrals, laterals, and cuspids.
- Class IV Caries affecting proximal including incisal edges of anterior teeth.
- Class V Caries affecting gingival 1/3 of facial or lingual surfaces of anterior or posterior teeth.
- Class VI Caries affecting cusp tips of molars, premolars, and cuspids.
Materials used
These casting alloys are mostly used for making crowns, bridges and dentures. Titanium, usually commercially pure but sometimes a 90% alloy, is used as the anchor for dental implants as it is biocompatible and can integrate into bone.
- Precious metallic alloys
- gold (high purity: 99.7%)
- gold alloys (with high gold content)
- gold-platina alloy
- silver-palladium alloy
- Base metallic alloys
- cobalt-chrome alloy
- nickel-chrome alloy
- Amalgam
- Silver amalgam (Consists of mercury (50%), silver (~22-32% ), tin (~14%), copper (~8%), and other trace metals)
Dental Amalgam is widely used because of the ease of fabricating the plastic material into rigid direct fillings, completed in single appointment, with acceptable strength, hardness, corrosion, and toxicity properties. It is more forgiving of preparation and technique than composite resins used for that purpose. It is now mainly used for posterior teeth. Although the mercury in cured amalgam is not available as free mercury, concern of its toxicity has existed since the invention of amalgam as a dental material. It is banned or restricted in Norway, Sweden and Finland. See Dental Amalgam Controversy.
- Direct Gold
- Gold
Although rarely used, due to expense and specialized training requirements, gold foil can be used for direct dental restorations.
Composite resin

Dental composites, also called "white fillings", are a group of restorative materials used in dentistry. Crowns and in-lays can be made in the laboratory from dental composites. These materials are similar to those used in direct fillings and are tooth-colored. Their strength and durability is not as high as porcelain or metal restorations and they are more prone to wear and discolouration. As with other composite materials, a dental composite typically consists of a resin-based matrix, such as a bisphenol A-glycidyl methacrylate (BISMA) resin like urethane dimethacrylate (UDMA), and an inorganic filler such as silica. Compositions vary widely, with proprietary mixes of resins forming the matrix, as well as engineered filler glasses and glass ceramics. The filler gives the composite wear resistance and translucency. A coupling agent such as silane is used to enhance the bond between these two components. An initiator package begins the polymerization reaction of the resins when external energy (light/heat, etc.) is applied.
After tooth preparation, a thin primer or bonding agent is used. Modern photo-polymerised composites are applied and cured in relatively thin layers as determined by their opacity.[4] After some curing, the final surface will be shaped and polished.
Glass ionomer cement
A glass ionomer cement (GIC) is one of a class of materials commonly used in dentistry as filling materials and luting cements. These materials are based on the reaction of silicate glass powder and polyalkenoic acid. These tooth-coloured materials were introduced in 1972 for use as restorative materials for anterior teeth (particularly for eroded areas, Class III and V cavities).
As they bond chemically to dental hard tissues and release fluoride for a relatively long period, modern-day applications of GICs have expanded. The desirable properties of glass ionomer cements make them useful materials in the restoration of carious lesions in low-stress areas such as smooth-surface and small anterior proximal cavities in primary teeth. Results from clinical studies also support the use of conventional glass ionomer restorations in primary molars. They need not be put in layer by layer, like in composite fillings.
Porcelain (ceramics)
Full-porcelain dental materials include Dental porcelain (porcelain meaning a high-firing-temperature ceramic), other ceramics, sintered-glass materials, and glass-ceramics as indirect fillings and crowns or metal-free "jacket crowns". They are also used as in-lays, on-lays, and aesthetic veneers. A veneer is a very thin shell of porcelain that can replace or cover part of the enamel of the tooth. Full-porcelain restorations are particularly desirable because their color and translucency mimic natural tooth enamel.
Another type is known as porcelain-fused-to-metal, which is used to provide strength to a crown or bridge. These restorations are very strong, durable and resistant to wear, because the combination of porcelain and metal creates a stronger restoration than porcelain used alone.
One of the advantages of computerized dentistry (CAD/CAM technologies) involves the use of machinable ceramics which are sold in a partially sintered, machinable state that is fired again after machining to form a hard ceramic. Some of the materials used are glass-bonded porcelain (Viablock), "lithium disilicate" glass-ceramic (a ceramic crystallizing from a glass by special heat treatment), and phase stabilized zirconia (zirconium dioxide, ZrO2). Previous attempts to utilize high-performance ceramics such as zirconium-oxide were thwarted by the fact that this material could not be processed using the traditional methods used in dentistry. Because of its high strength and comparatively much higher fracture toughness, sintered zirconium-oxide can be used in posterior crowns and bridges, implant abutments, and root dowel pins. Lithium disilicate (used in the latest Chairside Economical Restoration of Esthetic Ceramics CEREC product) also has the fracture resistance needed for use on molars.[6] Some all-ceramic restorations, such as porcelain-fused-to-alumina set the standard for high aesthetics in dentistry because they are strong and their color and translucency mimic natural tooth enamel. Not as aesthetic as porcelain-fused-to-ceramic, many dentists will not use new machine-made "monolithic" zirconia and lithium disilicate crowns on anterior (front) teeth.[7]
Cast metals and porcelain-on-metal are currently the standard material for crowns and bridges. The demand for full ceramic solutions, however, continues to grow.
Comparison
- Composites and Amalgam are used mainly for direct restoration. Composites can be made of color matching the tooth, and the surface can be polished after the filling procedure has been completed.
- Amalgam fillings expand with age, possibly cracking the tooth and requiring repair and filling replacement. But chance of leakage of filling is less.
- Composite fillings shrink with age and may pull away from the tooth allowing leakage. If leakage is not noticed early, recurrent decay may occur.
- A 2003 study showed that fillings have a finite lifespan: an average of 12.8 years for amalgam and 7.8 years for composite resins.[8] Fillings fail because of changes in the filling, tooth or the bond between them. Secondary cavity formation can also affect the structural integrity the original filling. Fillings are recommended for small to medium-sized restorations.
- Inlays and onlays are more expensive indirect restoration alternative to direct fillings. They are supposed to be more durable, but long-term studies did not always detect a significant lower failure rate of ceramic[9] or composite [10] inlays compared to composite direct fillings.
- Porcelain, cobalt-chrome, and gold are used for indirect restorations like crowns and partial coverage crowns (onlays). Traditional porcelains are brittle and are not always recommended for molar restorations. Some hard porcelains cause excessive wear on opposing teeth.
Experimental
The US National Institute of Dental Research and international organizations as well as commercial suppliers conduct research on new materials. In 2010, researchers reported that they were able to stimulate mineralization of an enamel-like layer of fluorapatite in vivo.[11] Filling material that is compatible with pulp tissue has been developed; it could be used where previously a root canal or extraction was required, according to 2016 reports.[12]
Socket preservation
Socket preservation is a procedure to reduce bone loss after tooth extraction to preserve the dental alveolus (tooth socket) in the alveolar bone. A platelet rich fibrin (PRF) membrane containing bone growth enhancing elements can be stitched over the wound or a graft material or scaffold is placed in the socket of an extracted tooth at the time of extraction. The socket is then directly closed with stitches or covered with a non-resorbable or resorbable membrane and sutured.
Restoration using dental implants
Dental implants are anchors placed in bone, usually made from titanium or titanium alloy. They can support dental restorations which replace missing teeth. Some restorative applications include supporting crowns, bridges, or dental prostheses.
See also
- Dental Curing Light
- Dental dam
- Dental treatment
- Fixed prosthodontics
- Gold teeth
- Treatment of knocked-out (avulsed) teeth
- Triodent V3 Sectional Matrix System for Class II restorations
References
- ↑ TCT magazine, "WorkNC Dental at the "CAD/CAM and Rapid Prototyping in Dental Technology" conference"
- ↑ G. V. Black Classification of Carious Lesions
- ↑ Dorfman J, The Center for Special Dentistry.
- ↑ Canadian Dental Association, Tooth-coloured fillings
- ↑ Dorfman J, The Center for Special Dentistry.
- ↑ Christian F.J. Stappert, Wael Att, Thomas Gerds, and Joerg R. Strub Fracture resistance of different partial-coverage ceramic molar restorations: An in vitro investigation J Am Dent Assoc 2006 137: 514-522.
- ↑ "Where and When Is It Appropriate to Place Monolithic vs. Layered Restorations," Inside Dentistry, August 2012, Vol. 8, Issue 8, E. McLaren, R. Margeas, N. Fahl.
- ↑ Van Nieuwenhuysen JP, D'Hoore W, Carvalho J, Qvist V (2003). "Long-term evaluation of extensive restorations in permanent teeth". Journal of Dentistry. 31 (6): 395–405. doi:10.1016/s0300-5712(03)00084-8. PMID 12878022.
- ↑ Clinical evaluation of ceramic inlays compared to composite restorations.; (2009); RT Lange, P Pfeiffer; Oper Dent. May-Jun;34(3):263-72. doi:10.2341/08-95
- ↑ Composite resin fillings and inlays. An 11-year evaluation.; U Pallesen, V Qvist; (2003) Clin Oral Invest 7:71–79 doi:10.1007/s00784-003-0201-z Conclusion:.." Considering the more invasive cavity preparation and the higher cost of restorations made by the inlay technique, this study indicates that resin fillings in most cases should be preferred over resin inlays."
- ↑ Guentsch et al. (2010). Biomimetic Mineralization: Effects on Human Enamel In Vivo. Advanced Engineering Materials.
- ↑ https://www.nottingham.ac.uk/news/pressreleases/2016/july/fillings-that-heal-your-teeth.aspx