Chorioamnionitis
| Chorioamnionitis | |
|---|---|
|
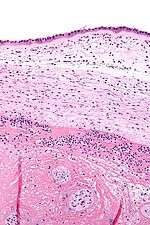
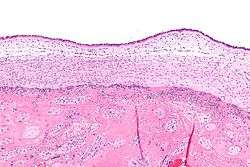
Micrograph showing chorioamnionitis. The clusters of blue dots are inflammatory cells (neutrophils, eosinophils and lymphocytes). H&E stain. | |
| Classification and external resources | |
| Specialty | Obstetrics gynecology |
| ICD-10 | O41.1, P02.7 |
| ICD-9-CM | 658.4, 762.7 |
| DiseasesDB | 31882 |
| eMedicine | ped/89 |
| MeSH | D002821 |
Chorioamnionitis also known as intra-amniotic infection (IAI)[1] is an inflammation of the fetal membranes (amnion and chorion) due to a bacterial infection. It typically results from bacteria ascending into the uterus from the vagina and is most often associated with prolonged labor. The risk of developing chorioamnionitis increases with each vaginal examination that is performed in the final month of pregnancy, including during labor.[3]
Background
The amniotic sac consists of two parts:
- The outer membrane is the chorion. It is closest to the mother and physically supports the much thinner amnion.
- The inner membrane is the amnion. It is in direct contact with the amniotic fluid, which surrounds the fetus.
Diagnosis
Clinical
Chorioamnionitis is diagnosed clinically in the setting of Maternal fever (≥ 100.4 °F) and at least two of the following: [2]
- Maternal leukocytosis (> 15,000 cells/mm³)
- Maternal tachycardia (> 100 bpm)
- Fetal tachycardia (> 160 bpm)
- Uterine tenderness
- Foul odor of amniotic fluid[3]
Exclusions:
- Maternal upper respiratory infection.
- Maternal urinary tract infection.
Pathologic
Chorioamnionitis can be diagnosed from a histologic examination of the fetal membranes.
Infiltration of the chorionic plate by neutrophils is diagnostic of (mild) chorioamnionitis. More severe chorioamnionitis involves subamniotic tissue and may have fetal membrane necrosis and/or abscess formation.
Severe chorioamnionitis may be accompanied by vasculitis of the umbilical blood vessels (due to the fetus' inflammatory cells) and, if very severe, funisitis (inflammation of the umbilical cord's connective tissue).
Treatment
Antibiotic Treatment consists of:
- Standard: Ampicillin 2g IV every 6 hours + Gentamicin 1.5 mg/kg every 8 hours
- Alternative: Ampicillin-Sulbactam 3g IV every 5 hours, Ticarcillin-Clavulanate 3.1g IV every 4 hours, Cefoxitine 2g IV every 6 hours
- Cesarean Delivery: Ampicillin 2g IV every 6 hours + Gentamicin 1.5 mg/kg every 8 hours + Clindamycin 900 mg every 8 hours or Metronidazole 500 mg IV every 6 hours
- Penicillin-Allergy: Vancomycin 1g IV every 12 hours + Gentamicin 1.5 mg/kg every 8 hours
Completion of treatment/cure is only considered after delivery.
Associations
Chorioamnionitis is a risk factor for periventricular leukomalacia and cerebral palsy.[5]
See also
Notes
- ↑ "Intra–Amniotic Infection". http://www.merckmanuals.com/. Retrieved 20 December 2014. External link in
|website=(help) - ↑ Elmar Peter Sakala, MD, MA, MPH, FACOG. Professor of GYNOB, Loma Linda University of medicine, California. Codirector of Student Clerkship. Dept of GYNOB
- ↑ http://www.uptodate.com/contents/intraamniotic-infection-chorioamnionitis
- ↑ http://www.uptodate.com/contents/intraamniotic-infection-chorioamnionitis
- ↑ Wu YW, Colford JM (2000). "Chorioamnionitis as a risk factor for cerebral palsy: A meta-analysis". JAMA. 284 (11): 1417–24. doi:10.1001/jama.284.11.1417. PMID 10989405.
References
- Excess Digital Exams Raise Risk of Chorioamnionitis, Ob.Gyn. News, August 15, 1997
- Centers for disease control and prevention (2002) Prevention of perinatal group B Streptococcal disease: revised guidelines from CDC. MMWR 51:RR-11:1–28
External links
- Overview at Cleveland Clinic.
- Cerebral palsy inflammation link (29 November 2003) at BBC.