Mitral valve
| Mitral valve | |
|---|---|
.svg.png)
 Anterior (frontal) view of the opened heart. White arrows indicate normal blood flow. (Mitral valve labeled at center right.) | |
 Base of ventricles exposed by removal of the atria. (Bicuspid (mitral) valve visible at bottom left.) | |
| Details | |
| Identifiers | |
| Latin |
Valva atrioventricularis sinistra, valva mitralis, valvula bicuspidalis |
| MeSH | A07.541.510.507 |
| TA | A12.1.04.003 |
| FMA | 7235 |
The mitral valve, also known as the bicuspid valve or left atrioventricular valve, is a dual-flap valve in the heart that lies between the left atrium and the left ventricle. The mitral valve (not to be confused with the congenital bicuspid aortic valve) and the tricuspid valve are known collectively as the atrioventricular valves because they lie between the atria and the ventricles of the heart and control the flow of blood.
During diastole, a normally-functioning mitral valve opens as a result of increased pressure from the left atrium as it fills with blood (preloading). As atrial pressure increases above that of the left ventricle, the mitral valve opens. Opening facilitates the passive flow of blood into the left ventricle. Diastole ends with atrial contraction, which ejects the final 20% of blood that is transferred from the left atrium to the left ventricle. This amount of blood is known as end-diastolic volume, and the mitral valve closes at the end of atrial contraction to prevent a reversal of blood flow.
Structure

The mitral valve is typically 4–6 cm² in area. It has two cusps, or leaflets (the anteromedial leaflet and the posterolateral leaflet), that guard the opening. The opening is surrounded by a fibrous ring known as the mitral valve annulus. (The orientation of the two leaflets resembles a bishop's mitre, whence the valve receives its name.[1]) The anterior cusp protects approximately two-thirds of the valve (imagine a crescent moon within the circle, where the crescent represents the posterior cusp). Although the anterior leaflet takes up a larger part of the ring and rises higher, the posterior leaflet has a larger surface area. These valve leaflets are prevented from prolapsing into the left atrium by the action of chordae tendineae, the tendons attached to the posterior surface of the valve.
The inelastic chordae tendineae are attached at one end to the papillary muscles and at the other to the valve cusps. Papillary muscles are finger-like projections from the wall of the left ventricle. Chordae tendineae from each muscle are attached to both leaflets of the mitral valve. Thus, when the left ventricle contracts, the intraventricular pressure forces the valve to close, while the tendons keep the leaflets coapting together and prevent the valve from opening in the wrong direction (thus preventing blood to flow back to the left atrium). Each chord has a different thickness. The thinnest ones are attached to the free leaflet margin, whereas thickest ones (strut chords) are attached quite away from the free margin. This disposition has important effects on systolic stress distribution physiology [2]
Function
During left ventricular diastole, after the pressure drops in the left ventricle due to relaxation of the ventricular myocardium, the mitral valve opens, and blood travels from the left atrium to the left ventricle. About 70 to 80% of the blood that travels across the mitral valve occurs during the early filling phase of the left ventricle. This early filling phase is due to active relaxation of the ventricular myocardium, causing a pressure gradient that allows a rapid flow of blood from the left atrium, across the mitral valve. This early filling across the mitral valve is seen on doppler echocardiography of the mitral valve as the E wave.
After the E wave, there is a period of slow filling of the ventricle.
Left atrial contraction (left atrial systole) (during left ventricular diastole) causes added blood to flow across the mitral valve immediately before left ventricular systole. This late flow across the open mitral valve is seen on doppler echocardiography of the mitral valve as the A wave. The late filling of the left ventricle contributes about 20% to the volume in the left ventricle prior to ventricular systole, and is known as the atrial kick.
The mitral annulus changes in shape and size during the cardiac cycle. It is smaller at the end of atrial systole due to the contraction of the left atrium around it, like a sphincter. This reduction in annulus size at the end of atrial systole may be important for the proper coapting of the leaflets of the mitral valve when the left ventricle contracts and pumps blood.[3] Leaking valves can be corrected by mitral valve annuloplasty, a common surgical procedure that aims at restoring proper leaflet adjustment.
Clinical significance

The closing of the mitral valve and the tricuspid valve constitutes the first heart sound (S1). It is not the valve closure itself which produces the sound but the sudden cessation of blood flow, when the mitral and tricuspid valves close.
There are some valvular heart diseases that affect the mitral valve. Mitral stenosis is a narrowing of the valve. This can be heard as an opening snap in a heart sound which is not normally present.
Classic mitral valve prolapse is caused by an excess of connective tissue that thickens the spongiosa layer of the cusp and separates collagen bundles in the fibrosa. This weakens the cusps and adjacent tissue, resulting in an increased cuspal area and lengthening of the chordae tendineae. Elongation of the chordae tendineae often causes rupture, commonly to the chordae attached to the posterior cusp. Advanced lesions—also commonly involving the posterior leaflet—lead to leaflet folding, inversion, and displacement toward the left atrium.[4]
A valve prolapse can result in mitral insufficiency which is a regurgitation or backflow of blood due to the incomplete closure of the valve. Surgery can be performed to replace or repair a damaged valve. A less invasive method is that of mitral valvuloplasty which uses a balloon catheter to open up a stenotic valve.
Mitral annulus

The mitral annulus is a fibrous ring that is attached to the mitral valve leaflets. Unlike prosthetic valves, it is neither circular nor continuous. The mitral annulus is saddle shaped and it is dynamic in shape throughout the cardiac cycle.[5] The annulus contracts and reduces its surface area during systole to help provide complete closure of the leaflets. Annular dilatation can result in poor leaflet apposition, leading to functional mitral regurgitation.[6]
The normal diameter of the mitral annulus is 3.1 ± 0.4 cm, and the circumference is 8 to 9 cm. There is no histologic evidence of an annular structure anteriorly, where the mitral valve leaflet is contiguous with the posterior aortic root.[7]
Rarely there can be a severe form known as caseous calcification of the mitral valve that can be mistaken for intracardiac mass or thrombus.[8]
Additional images
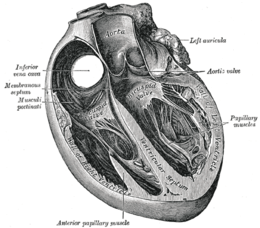 Section of the heart showing the ventricular septum. (Bicuspid valve visible at center.)
Section of the heart showing the ventricular septum. (Bicuspid valve visible at center.)
 Apical view of valves
Apical view of valves Cross-sectional view of mitral valve between left atrium (upper chamber) and left ventricle (lower chamber), which shows parts of walls of left atrium and left ventricle that are next to the mitral valve.
Cross-sectional view of mitral valve between left atrium (upper chamber) and left ventricle (lower chamber), which shows parts of walls of left atrium and left ventricle that are next to the mitral valve. Mitral valve
Mitral valve
Etymology and pronunciation
The word mitral (/ˈmaɪtrəl/) comes from Latin, meaning "shaped like a mitre" (bishop's hat). The word bicuspid uses combining forms of bi-, from Latin, meaning "double", and cusp, meaning "point", reflecting the dual-flap shape of the valve.
See also
References
- ↑ mitral valve, Stedman's Online Medical Dictionary at Lippincott Williams and Wilkins
- ↑ Nazari S, Carli F, Salvi S, et al. (Apr 2000). "Patterns of systolic stress distribution on mitral valve anterior leaflet chordal apparatus. A structural mechanical theoretical analysis". J Cardiovasc Surg (Torino). 41 (2): 193–202. PMID 10901521.
- ↑ Pai RG, Varadarajan P, Tanimoto M (2003). "Effect of atrial fibrillation on the dynamics of mitral annular area". The Journal of Heart Valve Disease. 12 (1): 31–7. PMID 12578332. Retrieved 2010-03-04.
- ↑ Playford, David; Weyman, Arthur (2001). "Mitral valve prolapse: time for a fresh look". Reviews in Cardiovascular Medicine. 2 (2): 73–81. PMID 12439384.
- ↑ Mahmood, Feroze; Shakil, Omair; Mahmood, Bilal; Chaudhry, Maria; Matyal, Robina; Khabbaz, Kamal R. (December 2013). "Mitral Annulus: An Intraoperative Echocardiographic Perspective". Journal of Cardiothoracic and Vascular Anesthesia. 27 (6): 1355–1363. doi:10.1053/j.jvca.2013.02.008.
- ↑ Perloff, JK; Roberts, WC (1972). "The mitral apparatus. Functional anatomy of mitral regurgitation". Circulation. 46 (2): 227–39. doi:10.1161/01.cir.46.2.227.
- ↑ Otto, Catherine M.; Robert Bonow (September 2009). Valvular Heart Disease: A Companion to Braunwald's Heart Disease. Elsevier Health Sciences. ISBN 1-4160-5892-3. External link in
|title=(help) - ↑ Kosior, Dariusz A. (2014). "Mitral annulus caseous calcification mimicking cardiac mass in asymptomatic patient – multimodality imaging approach to incidental echocardiographic finding". Polish Journal of Radiology. 79: 88–90. doi:10.12659/PJR.889830.
External links
- Anatomy figure: 20:07-03 at Human Anatomy Online, SUNY Downstate Medical Center — "Valves of the heart"
- Cardiac Valve Animations - Perioperative Interactive Education Group — Cardiac valve animations
Further reading
- Ingels, Jr, Neil B and Karlsson, Matts. Mitral Valve Mechanics. Linköping University Electronic Press, 2016. ISBN 978-91-7685-952-0. Open access