Prolonged grief disorder
Prolonged grief disorder (PGD) refers to a syndrome consisting of a distinct set of symptoms following the death of a loved one. PGD is relatively rare – experienced by about 10 percent[1] of bereaved survivors, though rates vary depending on the circumstances. The affected person is incapacitated by grief, so focused on the loss that it is difficult to care about much else. He or she often ruminates about the death and longs for a reunion with the departed, while feeling unsure of his or her own identity and place in the world. The victim will develop a flat and dull outlook on life, feeling that the future holds no prospect of joy, satisfaction or pleasure. The bereaved person who suffers from PGD feels devalued and in constant turmoil, with an inability to adjust to (if not a frank protest against) life without the beloved.
PGD is defined by its symptoms, duration and intensity. The symptoms are intense yearning for the person, identity confusion, difficulty accepting the loss, bitterness, emotional numbness, inability to trust others and the feeling of being trapped in grief. These are present every day, causing significant distress and functional impairment, and remaining intense, frequent, and disabling for six months or more after the death.[2]
Description
Grief is a normal response to bereavement. Researchers have found that 10–20%[1] of people experience a prolonged response to bereavement that impacts functioning and has adverse long-term effects on health.[3][4]
Prolonged grief is considered when an individual's ability to function and level of distress over the loss is extreme and persistent. People with PGD feel "stuck" in their grief, experience a chronic aching and yearning for the dear departed, feel that they are not the same person anymore (e.g., unsure of their identity, loss of a sense of self and self-worth), become emotionally disconnected from others, and lack the desire to "move on" (sometimes feeling that doing so would be betraying the person who is now deceased).[3][5][6][7][8][9][10]
History and discussion
The DSM-IV and ICD-10 do not distinguish between normal and prolonged grief.[11][12] Based on numerous findings of maladaptive effects of prolonged grief, diagnostic criteria for PGD have been proposed for inclusion in the DSM-5 and ICD-11.[3][13]
The proposed diagnostic criteria were the result of statistical analysis of a set of criteria agreed upon by a panel of experts.[3][10] The analyses produced criteria that were the most accurate markers of bereaved individuals suffering from painful, persistent, destructive PGD.[3] The criteria for PGD have been validated and dozens of studies both internationally and domestically are being conducted, and published, that validate the PGD criteria in other cultures, kinship relationships to the deceased and causes of death (e.g., earthquakes, tsunami, war, genocide, fires, bombings, palliative and acute care settings).[14][15]
Recognizing prolonged grief as a disorder would allow it to be better understood, detected, studied and treated. Insurance companies would also be more likely reimburse its care. On the other hand, inclusion of PGD in the DSM-5 and ICD-11 may be misunderstood as the medicalization of grief, reducing its dignity, turning love into pathology and implying that survivors should quickly forget and "get over" the loss. Bereaved persons may be insulted by having their distress labeled as a mental disorder. While this stigmatization would not be the intent, it might be an unintended consequence. In spite of this concern, studies have shown that nearly all bereaved individuals who met the criteria for PGD were receptive to treatment and their families relieved to know they had a recognizable syndrome.[16]
Difference from normal grief
Although extremely painful, grief is the normal process of accommodating to a new life without the deceased loved one. Most bereaved survivors manage to get through the worst of their grief and continue to function and find meaning in life. Normal grief differs from PGD in that it is not as intense, persistent, disabling and life-altering and is not experienced as a severe threat to the survivor's identity, sense of self-worth, feeling of security, safety or hopes for future happiness. Although normal grief remains with the bereaved person far into the future, its ability to disrupt the survivor's life dissipates with time.[2]
Diagnostic criteria
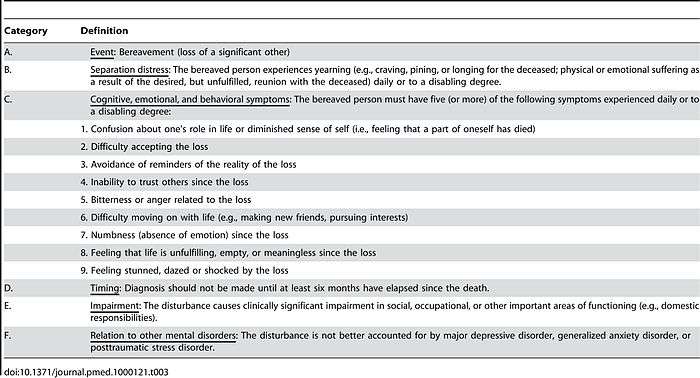
Factor analytic studies have determined that the symptoms of PGD form a unitary construct that is separate from symptoms of bereavement-related depression and anxiety.[3][3][5][6][7][9][10][17][18][19][20] Extensive research has been conducted to identify and isolate the symptoms that constitute PGD and distinguish it from diagnostic "nearest neighbors" such as Major Depressive Disorder or Posttraumatic Stress Disorder.[3][5][6][7][9][10][18][19][20] These analyses integrate clinical insights with rigorous empirical analysis to determine the set of symptoms that best indicate which bereaved survivors will be at risk of long term dysfunction and distress (e.g., suicidality, alcohol abuse, disability days, sleep impairment, quality of life impairment, high blood pressure, hospitalizations for serious medical events such as heart attacks).[3][5][8][9][21][22][23][24][25]
Prigerson et al. proposed diagnostic criteria for PGD for inclusion in the DSM-5 and ICD-11.[3]
Risk factors
Known risk factors and clinical correlates for PGD include a history of:
- Childhood separation anxiety[26]
- Controlling parents[27]
- Parental abuse or death[28]
- Close kinship relationship to the deceased (e.g., parents)[29][30]
- Insecure attachment styles[31]
- Emotional dependency[31][32]
- Lack of preparation for death[33][34]
- Death in hospital[35]
- No shortened rapid eye movement (REM) latency[36]
- Activation of the nucleus accumbens[37]
These risk factors and clinical correlates have been shown to relate to PGD symptoms and not symptoms of Major Depressive Disorder (MDD), Post-traumatic Stress Disorder (PTSD), and Generalized Anxiety Disorder (GAD).[26][36]
Health consequences
PGD symptoms have been associated with:
- Elevated rates of suicidal ideation and attempts[9]
- Cancer[8]
- Immunological dysfunction[38]
- Hypertension[8]
- Cardiac events[8]
- Functional impairment[3][8]
- Adverse health behaviors[8]
- Reduced quality of life in adults[5][8][9][21][22][23] and in children[38]
- Increased health service use and sick leave[25]
Treatment
The unique symptom profile and course of PGD requires targeted treatment. Randomized control trials (RCT) have proven tricyclic antidepressants alone or together with interpersonal psychotherapy ineffective in reducing PGD symptoms, while psychotherapy designed specifically for PGD has been proven to be beneficial.[39][40][41][42][43] Preliminary results of an online, self-management intervention to prevent PGD in recently bereaved individuals, in a study called "HEAL" (Healthy Experiences After Loss), are very promising.[44] A larger randomized controlled trial is being planned.
Incidence
Out of the people surveyed who have experienced a loss, 10–20% display a prolonged and severe grief response.[3][4] Global incidence needs further investigation.
References
- 1 2 Davis, Mellar; Feyer, Petra; Ortner, Petra; Zimmermann, Camilla (2011). Supportive Oncology. Philadelphia, PA: Elsevier Saunders. p. 628. ISBN 978-1-4377-1015-1.
- 1 2 Frances, A. (2012, February 28). When Good Grief Goes Bad. The Huffington Post. Retrieved from http://www.huffingtonpost.com/allen-frances/grief-depression_b_1301050.html
- 1 2 3 4 5 6 7 8 9 10 11 12 Prigerson, Holly G.; Horowitz, Mardi J.; Jacobs, Selby C.; Parkes, Colin M.; Aslan, Mihaela; Goodkin, Karl; Raphael, Beverley; Marwit, Samuel J.; et al. (2009). Brayne, Carol, ed. "Prolonged Grief Disorder: Psychometric Validation of Criteria Proposed for DSM-V and ICD-11". PLoS Medicine. 6 (8): e1000121. doi:10.1371/journal.pmed.1000121. PMC 2711304
 . PMID 19652695.
. PMID 19652695. - 1 2 Prigerson, Holly G.; Vanderwerker, Lauren C.; Maciejewski, Paul K. (2008). "A case for inclusion of prolonged grief disorder in DSM-5". In Stroebe, Margaret S.; Hansson, Robert O.; Schut, Henk; et al. Handbook of Bereavement Research and Practice: Advances in Theory and intervention. Washington, DC: American Psychological Association. pp. 165–86. ISBN 978-1-4338-0351-2.
- 1 2 3 4 5 Prigerson, HG; Frank, E; Kasl, SV; Reynolds, CF; Anderson, B; Zubenko, GS; Houck, PR; George, CJ; Kupfer, DJ (1995). "Complicated grief and bereavement-related depression as distinct disorders: Preliminary empirical validation in elderly bereaved spouses". The American Journal of Psychiatry. 152 (1): 22–30. PMID 7802116.
- 1 2 3 Prigerson, Holly G.; MacIejewski, Paul K.; Reynolds, Charles F.; Bierhals, Andrew J.; Newsom, Jason T.; Fasiczka, Amy; Frank, Ellen; Doman, Jack; Miller, Mark (1995). "Inventory of complicated grief: A scale to measure maladaptive symptoms of loss". Psychiatry Research. 59 (1–2): 65–79. doi:10.1016/0165-1781(95)02757-2. PMID 8771222.
- 1 2 3 Prigerson, HG; Bierhals, AJ; Kasl, SV; Reynolds, CF; Shear, MK; Newsom, JT; Jacobs, S (1996). "Complicated grief as a disorder distinct from bereavement-related depression and anxiety: A replication study". The American Journal of Psychiatry. 153 (11): 1484–6. PMID 8890686.
- 1 2 3 4 5 6 7 8 Prigerson, HG; Bierhals, AJ; Kasl, SV; Reynolds, CF; Shear, MK; Day, N; Beery, LC; Newsom, JT; Jacobs, S (1997). "Traumatic grief as a risk factor for mental and physical morbidity". The American Journal of Psychiatry. 154 (5): 616–23. PMID 9137115.
- 1 2 3 4 5 6 Prigerson, HG; Bridge, J; MacIejewski, PK; Beery, LC; Rosenheck, RA; Jacobs, SC; Bierhals, AJ; Kupfer, DJ; Brent, DA (1999). "Influence of traumatic grief on suicidal ideation among young adults". The American Journal of Psychiatry. 156 (12): 1994–5. PMID 10588419.
- 1 2 3 4 Prigerson, H. G.; Shear, M. K.; Jacobs, S. C.; Reynolds, C. F.; MacIejewski, P. K.; Davidson, J. R.; Rosenheck, R.; Pilkonis, P. A.; Wortman, C. B.; Williams, J. B.; Widiger, T. A.; Frank, E.; Kupfer, D. J.; Zisook, S. (1999). "Consensus criteria for traumatic grief. A preliminary empirical test". The British Journal of Psychiatry. 174: 67–73. doi:10.1192/bjp.174.1.67. PMID 10211154.
- ↑ American Psychiatric Association (1994). Diagnostic and statistical manual of mental disorders: DSM-IV (4th ed.). Washington: American Psychiatric Press. ISBN 0-89042-062-9.
- ↑ National Center for Health Statistics (2009) International Classification of Diseases, Tenth Revision (ICD-10).; Available at: CDC. Accessed 12 July 2012.
- ↑ Boelen, Paul A.; Prigerson, Holly G. (2012). "Commentary to the inclusion of Persistent Complex Bereavement-Related Disorder in DSM-5". Death Studies.
- ↑ Rodriguez Villar, S.; Sanchez Casado, M.; Prigerson, H. G.; Mesa Garcia, S.; Rodriguez Villar, M.; Hortiguela Martin, V. A.; Marco Schulke, C. M.; Barrientos Vega, R.; Quintana, M. (2012). "Prolonged Grief Disorder in the Next of Kin of Adult Patients Who Die During or After Admission to Intensive Care". Chest. 141 (6): 1635–6. doi:10.1378/chest.11-3099. PMID 22670028.
- ↑ Morina, Nexhmedin; Von Lersner, Ulrike; Prigerson, Holly G. (2011). Laks, Jerson, ed. "War and Bereavement: Consequences for Mental and Physical Distress". PLoS ONE. 6 (7): e22140. doi:10.1371/journal.pone.0022140. PMC 3134481
 . PMID 21765944.
. PMID 21765944. - ↑ Johnson, Jeffrey G.; First, Michael B.; Block, Susan; Vanderwerker, Lauren C.; Zivin, Kara; Zhang, Baohui; Prigerson, Holly G. (2009). "Stigmatization and Receptivity to Mental Health Services Among Recently Bereaved Adults". Death Studies. 33 (8): 691–711. doi:10.1080/07481180903070392. PMC 2834798
 . PMID 19697482.
. PMID 19697482. - ↑ Simon, Naomi M.; Wall, Melanie M.; Keshaviah, Aparna; Dryman, M. Taylor; Leblanc, Nicole J.; Shear, M. Katherine (2011). "Informing the symptom profile of complicated grief". Depression and Anxiety. 28 (2): 118–26. doi:10.1002/da.20775. PMC 3079952
 . PMID 21284064.
. PMID 21284064. - 1 2 Boelen, P. A.; Van Den Bout, J (2005). "Complicated Grief, Depression, and Anxiety as Distinct Postloss Syndromes: A Confirmatory Factor Analysis Study". American Journal of Psychiatry. 162 (11): 2175–7. doi:10.1176/appi.ajp.162.11.2175. PMID 16263861.
- 1 2 Boelen, P. A.; Van Den Bout, J; De Keijser, J (2003). "Traumatic Grief as a Disorder Distinct from Bereavement-Related Depression and Anxiety: A Replication Study with Bereaved Mental Health Care Patients". American Journal of Psychiatry. 160 (7): 1339–41. doi:10.1176/appi.ajp.160.7.1339. PMID 12832252.
- 1 2 MacIejewski, Paul K.; Zhang, B; Block, SD; Prigerson, HG (2007). "An Empirical Examination of the Stage Theory of Grief". JAMA. 297 (7): 716–23. doi:10.1001/jama.297.7.716. PMID 17312291.
- 1 2 Latham, Amy E.; Prigerson, Holly G. (2004). "Suicidality and Bereavement: Complicated Grief as Psychiatric Disorder Presenting Greatest Risk for Suicidality". Suicide and Life-Threatening Behavior. 34 (4): 350–62. doi:10.1521/suli.34.4.350.53737. PMC 1459278
 . PMID 15585457.
. PMID 15585457. - 1 2 Jacobsen, Julietc; Vanderwerker, Laurenc; Block, Susand; Friedlander, Robertj; MacIejewski, Paulk; Prigerson, Hollyg (2006). "Depression and demoralization as distinct syndromes: Preliminary data from a cohort of advanced cancer patients". Indian Journal of Palliative Care. 12: 8–15. doi:10.4103/0973-1075.25913.
- 1 2 Silverman, G. K.; Jacobs, S. C.; Kasl, S. V.; Shear, M. K.; MacIejewski, P. K.; Noaghiul, F. S.; Prigerson, H. G. (2000). "Quality of life impairments associated with diagnostic criteria for traumatic grief". Psychological Medicine. 30 (4): 857–62. doi:10.1017/S0033291799002524. PMID 11037094.
- ↑ Melhem, Nadine M.; Moritz, Grace; Walker, Monica; Shear, M. Katherine; Brent, David (2007). "Phenomenology and Correlates of Complicated Grief in Children and Adolescents". Journal of the American Academy of Child & Adolescent Psychiatry. 46 (4): 493–499. doi:10.1097/chi.0b013e31803062a9.
- 1 2 Lannen, P. K.; Wolfe, J.; Prigerson, H. G.; Onelov, E.; Kreicbergs, U. C. (2008). "Unresolved Grief in a National Sample of Bereaved Parents: Impaired Mental and Physical Health 4 to 9 Years Later". Journal of Clinical Oncology. 26 (36): 5870–6. doi:10.1200/JCO.2007.14.6738. PMC 2645112
 . PMID 19029425.
. PMID 19029425. - 1 2 Vanderwerker, Lauren C.; Jacobs, Selby C.; Parkes, Colin Murray; Prigerson, Holly G. (2006). "An Exploration of Associations Between Separation Anxiety in Childhood and Complicated Grief in Later Life". The Journal of Nervous and Mental Disease. 194 (2): 121–3. doi:10.1097/01.nmd.0000198146.28182.d5. PMID 16477190.
- ↑ Johnson, Jeffrey G.; Zhang, Baohui; Greer, Joseph A.; Prigerson, Holly G. (2007). "Parental Control, Partner Dependency, and Complicated Grief Among Widowed Adults in the Community". The Journal of Nervous and Mental Disease. 195 (1): 26–30. doi:10.1097/01.nmd.0000252009.45915.b2. PMID 17220736.
- ↑ Silverman, GK; Johnson, JG; Prigerson, HG (2001). "Preliminary explorations of the effects of prior trauma and loss on risk for psychiatric disorders in recently widowed people". The Israel Journal of Psychiatry and Related Sciences. 38 (3–4): 202–15. PMID 11725418.
- ↑ Mitchell, Ann M.; Kim, Yookyung; Prigerson, Holly G.; Mortimer-Stephens, Marykay (2004). "Complicated Grief in Survivors of Suicide". Crisis: the Journal of Crisis Intervention and Suicide Prevention. 25: 12–18. doi:10.1027/0227-5910.25.1.12.
- ↑ Cleiren, M; Diekstra, RF; Kerkhof, AJ; Van Der Wal, J (1994). "Mode of death and kinship in bereavement: Focusing on "who" rather than "how"". Crisis. 15 (1): 22–36. PMID 8062585.
- 1 2 Van Doorn, Carol; Kasl, Stanislav V.; Beery, Laurel C.; Jacobs, Selby C.; Prigerson, Holly G. (1998). "The Influence of Marital Quality and Attachment Styles on Traumatic Grief and Depressive Symptoms". The Journal of Nervous & Mental Disease. 186 (9): 566–573. doi:10.1097/00005053-199809000-00008.
- ↑ Johnson, Jeffrey G.; Vanderwerker, Lauren C.; Bornstein, Robert F.; Zhang, Baohui; Prigerson, Holly G. (2006). "Development and Validation of an Instrument for the Assessment of Dependency Among Bereaved Persons". Journal of Psychopathology and Behavioral Assessment. 28 (4): 261–70. doi:10.1007/s10862-005-9016-3.
- ↑ Barry, L. C.; Kasl, SV; Prigerson, HG (2002). "Psychiatric Disorders Among Bereaved Persons: The Role of Perceived Circumstances of Death and Preparedness for Death". American Journal of Geriatric Psychiatry. 10 (4): 447–57. doi:10.1176/appi.ajgp.10.4.447. PMID 12095904.
- ↑ Hebert, Randy S.; Dang, Qianyu; Schulz, Richard (2006). "Preparedness for the Death of a Loved One and Mental Health in Bereaved Caregivers of Patients with Dementia: Findings from the REACH Study". Journal of Palliative Medicine. 9 (3): 683–93. doi:10.1089/jpm.2006.9.683. PMID 16752974.
- ↑ Wright, A. A.; Keating, N. L.; Balboni, T. A.; Matulonis, U. A.; Block, S. D.; Prigerson, H. G. (2010). "Place of Death: Correlations with Quality of Life of Patients with Cancer and Predictors of Bereaved Caregivers' Mental Health". Journal of Clinical Oncology. 28 (29): 4457–64. doi:10.1200/JCO.2009.26.3863. PMC 2988637
 . PMID 20837950.
. PMID 20837950. - 1 2 McDermott, Owen D.; Prigerson, Holly G.; Reynolds, Charles F.; Houck, Patricia R.; Dew, Mary Amanda; Hall, Martica; Mazumdar, Sati; Buysse, Daniel J.; et al. (1997). "Sleep in the wake of complicated grief symptoms: An exploratory study". Biological Psychiatry. 41 (6): 710–6. doi:10.1016/S0006-3223(96)00118-7. PMID 9066995.
- ↑ O'Connor, Mary-Frances; Wellisch, David K.; Stanton, Annette L.; Eisenberger, Naomi I.; Irwin, Michael R.; Lieberman, Matthew D. (2008). "Craving love? Enduring grief activates brain's reward center". NeuroImage. 42 (2): 969–72. doi:10.1016/j.neuroimage.2008.04.256. PMC 2553561
 . PMID 18559294.
. PMID 18559294. - 1 2 Irwin M, Daniels M, Weiner H (1987). "Immune and neuroendocrine changes during bereavement". Psychiatr Clin North Am. 10: 449–465.
- ↑ Reynolds, CF; Miller, MD; Pasternak, RE; Frank, E; Perel, JM; Cornes, C; Houck, PR; Mazumdar, S; et al. (1999). "Treatment of bereavement-related major depressive episodes in later life: A controlled study of acute and continuation treatment with nortriptyline and interpersonal psychotherapy". The American Journal of Psychiatry. 156 (2): 202–8. PMID 9989555.
- ↑ Jacobs, SC; Nelson, JC; Zisook, S (1987). "Treating depressions of bereavement with antidepressants. A pilot study". The Psychiatric clinics of North America. 10 (3): 501–10. PMID 3684751.
- ↑ Pasternak, RE; Reynolds, CF; Schlernitzauer, M; Hoch, CC; Buysse, DJ; Houck, PR; Perel, JM (1991). "Acute open-trial nortriptyline therapy of bereavement-related depression in late life". The Journal of Clinical Psychiatry. 52 (7): 307–10. PMID 2071562.
- ↑ Shear, K.; Frank, Ellen; Houck, Patricia R.; Reynolds, Charles F. (2005). "Treatment of Complicated Grief: A Randomized Controlled Trial". JAMA: the Journal of the American Medical Association. 293 (21): 2601. doi:10.1001/jama.293.21.2601.
- ↑ Boelen, Paul A.; De Keijser, Jos; Van Den Hout, Marcel A.; Van Den Bout, Jan (2007). "Treatment of complicated grief: A comparison between cognitive-behavioral therapy and supportive counseling". Journal of Consulting and Clinical Psychology. 75 (2): 277–84. doi:10.1037/0022-006X.75.2.277. PMID 17469885.
- ↑ Clinical trial number NCT00598884 for "Effectiveness of an Internet-Based Self-Management Program in Treating Prolonged Grief Disorder" at ClinicalTrials.gov