Cat-scratch disease
| Cat scratch disease | |
|---|---|
| cat-scratch fever, Teeny's disease, inoculation lymphoreticulosis, subacute regional lymphadenitis[1] | |
|
| |
| Classification and external resources | |
| Specialty | Infectious disease |
| ICD-10 | A28.1 |
| ICD-9-CM | 078.3 |
| DiseasesDB | 2173 |
| MedlinePlus | 001614 |
| eMedicine | emerg/84 |
| Patient UK | Cat-scratch disease |
| MeSH | D002372 |
Cat-scratch disease (CSD) is a common and usually benign infectious disease caused by the bacterium Bartonella henselae.[2][3] It is most commonly found in children following a scratch or bite from a cat[2] within about one to two weeks.
Signs and symptoms
Cat-scratch disease commonly presents as tender, swollen lymph nodes near the site of the inoculating bite or scratch or on the neck, and is usually limited to one side. This condition is referred to as regional lymphadenopathy and occurs 1–3 weeks after inoculation.[4] Lymphadenopathy in CSD most commonly occurs in the arms, neck, or jaw, but may also occur near the groin or around the ear.[2] A vesicle or an erythematous papule may form at the site of initial infection.[2] Most patients also develop systemic symptoms such as malaise, decreased appetite, and aches.[2] Other associated complaints include headache, chills, muscular pains, joint pains, arthritis, backache, and abdominal pain. It may take 7 to 14 days, or as long as two months, for symptoms to appear. Most cases are benign and self-limiting, but lymphadenopathy may persist for several months after other symptoms disappear.[2] The disease usually resolves spontaneously, with or without treatment, in one month.
In rare situations, CSD can lead to the development of serious neurologic or cardiac sequelae such as meningoencephalitis, encephalopathy, seizures, or endocarditis.[2] Endocarditis associated with Bartonella infection has a particularly high mortality.[4] Parinaud's oculoglandular syndrome is the most common ocular manifestation of CSD,[2] and is a granulomatous conjunctivitis with concurrent swelling of the lymph node near the ear.[5] Optic neuritis or neuroretinitis is one of the atypical presentations.[6]
Immunocompromised patients are susceptible to other conditions associated with B. henselae and B. quintana, such as bacillary angiomatosis or bacillary peliosis.[2] Bacillary angiomatosis is primarily a vascular skin lesion that may extend to bone or be present in other areas of the body. In the typical scenario, the patient has HIV or another cause of severe immune dysfunction. Bacillary peliosis is caused by B. henselae that most often affects patients with HIV and other conditions causing severe immune compromise. The liver and spleen are primarily affected, with findings of blood-filled cystic spaces on pathology.[7] In 2015 a Toledo, Ohio woman lost eyesight in an eye after a cat licked it.[8]
Cause
Bartonella henselae is a fastidious,[4] intracellular, Gram-negative bacteria.
Transmission
The cat was recognized as the natural reservoir of the disease in 1950 by Robert Debré.[4] Kittens are more likely to carry the bacteria in their blood, and therefore may be more likely to transmit the disease than adult cats. However, fleas serve as a vector for transmission of B. henselae among cats,[4] and viable B. henselae are excreted in the feces of Ctenocephalides felis, the cat flea.[9] Cats could be infected with B. henselae through intradermal inoculation using flea feces containing B. henselae.[10] As a consequence, a likely means of transmission of B. henselae from cats to humans may be inoculation with flea feces containing B. henselae through a contaminated cat scratch wound or by cat saliva transmitted in a bite.[4] Ticks can also act as vectors and occasionally transmit the bacteria to humans.[2] Combined clinical and PCR-based research has shown that other organisms can transmit Bartonella, including spiders.[11][12] Cryptic Bartonella infection may be a much larger problem than previously thought, constituting an unrecognized occupational health hazard of veterinarians.,[13]
Diagnosis
The Warthin–Starry stain can be helpful to show the presence of B. henselae, but is often difficult to interpret. B. henselae is difficult to culture and can take 2–6 weeks to incubate.[4] The best diagnostic method currently available is polymerase chain reaction, which has a sensitivity of 43-76% and a specificity (in one study) of 100%.[4]
Histology
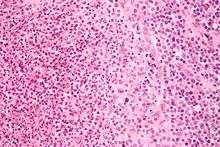
Cat-scratch disease is characterized by granulomatous inflammation on histological examination of the lymph nodes. Under the microscope, the skin lesion demonstrates a circumscribed focus of necrosis, surround by histiocytes, often accompanied by multinucleated giant cells, lymphocytes, and eosinophils. The regional lymph nodes demonstrate follicular hyperplasia with central stellate necrosis with neutrophils, surrounded by palisading histiocytes (suppurative granulomas) and sinuses packed with monocytoid B cells, usually without perifollicular and intrafollicular epithelioid cells. This pattern, although typical, is only present in a minority of cases.[14]
Treatment
Most healthy people clear the infection without treatment, but in 5 to 14 percent of individuals, the organisms disseminate and infect the liver, spleen, eye, or central nervous system.[15] Although some experts recommend not treating typical CSD in immunocompetent patients with mild to moderate illness, treatment of all patients with antimicrobial agents (Grade 2B) is suggested due to the probability of disseminated disease. The preferred antibiotic for treatment is azithromycin since this agent is the only one studied in a randomized controlled study.[16]
Azithromycin is preferentially used in pregnancy to avoid the teratogenic side effects of doxycycline.[17] However, doxycycline is preferred to treat B. henselae infections with optic neuritis due to its ability to adequately penetrate the tissues of the eye and central nervous system.[4]
Prevention
Cat-scratch disease can be primarily prevented by taking flea control measures and washing hands after handling a cat or cat feces; since cats are mostly exposed to fleas when they are outside, keeping cats inside can prevent infestation.[18]
Epidemiology
Bartonella henselae is found worldwide and CSD has been observed in many countries. The incidence of CSD appears to have a seasonal relationship, possibly due to the mating behavior of the cat flea during certain times of the year.[4]
History
Symptoms similar to CSD were first described by Henri Parinaud in 1889, and the clinical syndrome was first described in 1950 by Robert Debré.[3][4] In 1983, the Warthin-Starry silver stain was used to discover a Gram-negative bacillus which was named Afipia felis in 1991 after it was successfully cultured and isolated. The causative organism of CSD was originally believed to be Afipia felis, but this was disproved by immunological studies in the 1990s demonstrating that cat-scratch fever patients developed antibodies to two other organisms, B. henselae (originally known as Rochalimea henselae before the genera Bartonella and Rochalimea were combined) and B. clarridgeiae, which is a rod-shaped Gram-negative bacterium.[4]
References
- ↑ Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 1-4160-2999-0.
- 1 2 3 4 5 6 7 8 9 10 Klotz SA, Ianas V, Elliott SP (2011). "Cat-scratch Disease". American Family Physician. 83 (2): 152–5. PMID 21243990.
- 1 2 Asano S (2012). "Granulomatous lymphadenitis". Journal of Clinical and Experimental Hematopathology. 52 (1): 1–16. doi:10.3960/jslrt.52.1. PMID 22706525.
- 1 2 3 4 5 6 7 8 9 10 11 12 Florin TA, Zaoutis TE, Zaoutis LB (2008). "Beyond cat scratch disease: widening spectrum of Bartonella henselae infection". Pediatrics. 121 (5): e1413–25. doi:10.1542/peds.2007-1897. PMID 18443019.
- ↑ Catscratch Disease~clinical at eMedicine
- ↑ Gajula V, Kamepalli R, Kalavakunta JK (2014). "A star in the eye: cat scratch neuroretinitis". Clinical Case Reports. 2 (1): 17. doi:10.1002/ccr3.43. PMC 4184768
 . PMID 25356231.
. PMID 25356231. - ↑ Perkocha LA, Geaghan SM, Yen TS, Nishimura SL, Chan SP, Garcia-Kennedy R, Honda G, Stoloff AC, Klein HZ, Goldman RL (1990). "Clinical and pathological features of bacillary peliosis hepatis in association with human immunodeficiency virus infection". The New England Journal of Medicine. 323 (23): 1581–6. doi:10.1056/NEJM199012063232302. PMID 2233946.
- ↑ Tuey, Holly; Kinsey, Andrew (May 28, 2015). "Woman loses eyesight after her cat licks her". WTOL.
- ↑ Higgins JA, Radulovic S, Jaworski DC, Azad AF (1996). "Acquisition of the cat scratch disease agent Bartonella henselae by cat fleas (Siphonaptera:Pulicidae)". Journal of Medical Entomology. 33 (3): 490–5. doi:10.1093/jmedent/33.3.490. PMID 8667399.
- ↑ Foil L, Andress E, Freeland RL, Roy AF, Rutledge R, Triche PC, O'Reilly KL (1998). "Experimental infection of domestic cats with Bartonella henselae by inoculation of Ctenocephalides felis (Siphonaptera: Pulicidae) feces". Journal of Medical Entomology. 35 (5): 625–8. doi:10.1093/jmedent/35.5.625. PMID 9775583.
- ↑ Copeland, Claudia S. (2015). "Cat Scratch Fever? Really?: Cats, Fleas and the Many Faces of Bartonellosis". Healthcare Journal of Baton Rouge: 28–34.
- ↑ Mascarelli PE, Maggi RG, Hopkins S, Mozayeni BR, Trull CL, Bradley JM, Hegarty BC, Breitschwerdt EB (2013). "Bartonella henselae infection in a family experiencing neurological and neurocognitive abnormalities after woodlouse hunter spider bites". Parasites & Vectors. 6: 98. doi:10.1186/1756-3305-6-98. PMC 3639822
 . PMID 23587343.
. PMID 23587343. - ↑ Lantos PM, Maggi RG, Ferguson B, Varkey J, Park LP, Breitschwerdt EB, Woods CW (2014). "Detection of Bartonella species in the blood of veterinarians and veterinary technicians: a newly recognized occupational hazard?". Vector Borne and Zoonotic Diseases. 14 (8): 563–70. doi:10.1089/vbz.2013.1512. PMC 4117269
 . PMID 25072986.
. PMID 25072986. - ↑ Rosado FG, Stratton CW, Mosse CA (2011). "Clinicopathologic correlation of epidemiologic and histopathologic features of pediatric bacterial lymphadenitis". Archives of Pathology & Laboratory Medicine. 135 (11): 1490–3. doi:10.5858/arpa.2010-0581-OA. PMID 22032579.
- ↑ Carithers, H. A. (1985-11-01). "Cat-scratch disease. An overview based on a study of 1,200 patients". American Journal of Diseases of Children (1960). 139 (11): 1124–1133. doi:10.1001/archpedi.1985.02140130062031. ISSN 0002-922X. PMID 4061408.
- ↑ Rolain, J. M.; Brouqui, P.; Koehler, J. E.; Maguina, C.; Dolan, M. J.; Raoult, D. (2004-06-01). "Recommendations for Treatment of Human Infections Caused by Bartonella Species". Antimicrobial Agents and Chemotherapy. 48 (6): 1921–1933. doi:10.1128/AAC.48.6.1921-1933.2004. ISSN 0066-4804. PMC 415619
 . PMID 15155180.
. PMID 15155180. - ↑ Catscratch Disease~treatment at eMedicine
- ↑ Nelson, Christina A.; Saha, Shubhayu; Mead, Paul S. "Cat-Scratch Disease in the United States, 2005–2013". Emerging Infectious Diseases. 22 (10): 1741–1746. doi:10.3201/eid2210.160115.
External links
- Cat Scratch Disease on National Organization for Rare Disorders site
- Cat Scratch Fever Disease
- Cat Scratch Fever
